You felt pressure in your jaw long before any real pain appeared
It wasn’t sharp. Just pressure. Somewhere near the back of your mouth. You assumed it was nothing. Maybe stress. Maybe clenching. But it didn’t leave. Days passed. Then weeks. And now chewing feels different. You press your tongue back and something resists. Something that never broke the surface.
The tooth never erupted, but your discomfort kept growing anyway
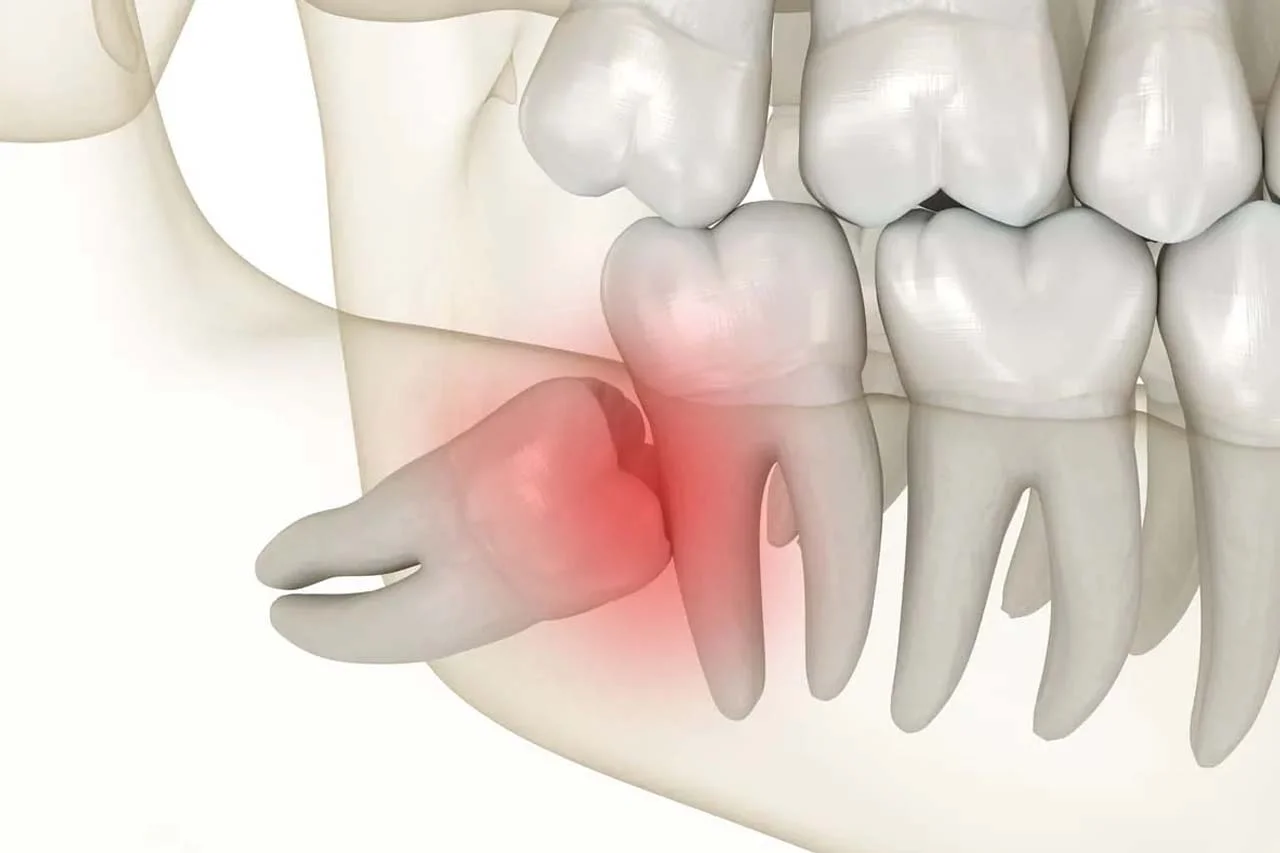
You expected a tooth to appear. A molar. Maybe a wisdom tooth. But nothing came. Just discomfort. A low throb at night. A dull ache after meals. Your dentist mentions impaction. A tooth that’s trapped. Not just under gum, but often bone. It’s not growing in the right direction. Sometimes sideways. Sometimes stalled completely.
X-rays reveal the tooth isn’t just stuck—it’s crowding the rest of your teeth silently
You thought it was isolated. But then you saw the scan. The hidden tooth pushing others. Slowly. Quietly. Creating tension across your whole bite. It’s not just about eruption. It’s about pressure. Alignment. And potential long-term damage. Impacted teeth don’t always scream. But they disturb the structure beneath the surface.
Wisdom teeth are the usual suspects, but they’re not the only ones
Third molars lead the list. Most people know that. But any tooth can be impacted. Canines, premolars, even incisors. Sometimes there’s not enough space. Sometimes the gumline hardens too early. Other times, the tooth forms in the wrong position from the start. What matters most is not just the tooth—but the direction it’s heading.
You notice headaches more frequently, and you didn’t link them to your jaw until now
The jaw is quiet but powerful. Misalignment affects everything above it. Tension builds. Muscles tighten. Nerves respond. Impacted teeth can contribute to headaches. Even earaches. Because the jaw is close to many delicate systems. The pressure radiates. And often, it’s misattributed to unrelated causes.
The gum around the area becomes swollen or red, and sometimes bleeds when brushing
It’s not always pain that signals the problem. Sometimes it’s the gum. It reacts first. Swells. Bleeds. Traps food. You feel tenderness without an open wound. That’s inflammation. Caused by a tooth trying—and failing—to erupt. Left untreated, it invites bacteria. That leads to infection. Or worse, a cyst.
Your dentist refers you to an oral surgeon, and now the word ‘extraction’ is on the table
The general checkup became a referral. Suddenly, you’re in a surgical chair. Not today, but soon. The surgeon explains angles. Roots. Risks. And the safest ways to remove what’s hidden. Impacted teeth often don’t come out like others. They require incisions. Sometimes bone removal. Sometimes sectioning the tooth into smaller parts.
Surgical extraction is precise, but it’s not without healing time and post-op care
You’re numbed. Or sedated. The tooth is removed, but healing takes attention. Days of swelling. Soft foods. Ice packs. Gentle rinsing. Avoiding straws. Maybe antibiotics. Maybe stitches. You expect soreness. But what you might not expect is relief. Because the pressure fades. The space is restored. The mouth feels balanced again.
Sometimes, orthodontic assistance is used to guide impacted teeth into place, rather than remove them
Not all impacted teeth must be removed. Especially canines. If the root is strong and angle correctable, braces can guide eruption. A surgical window exposes the tooth. A bracket is attached. Gentle pressure is applied over months. It’s not quick. But it saves the tooth. And it protects your natural bite.
Leaving an impacted tooth untreated can cause bone damage, infections, or even neighboring tooth loss
Avoidance doesn’t neutralize risk. An impacted tooth may seem silent now. But it erodes over time. Bone around it weakens. Infection risks grow. Teeth next to it may shift or decay. That’s why early imaging matters. Not to panic—but to plan. Because surgery delayed often becomes surgery complicated.
